Common Questions About ALTCS / Arizona Medicaid
What is the difference between ALTCS – Arizona Long-Term Care System and AHCCCS – Arizona Health Care Cost Containment System?
AHCCCS provides managed health care benefits through various health care providers or HMOs.
Through the HMOs, AHCCCS provides benefits for hospitalization, emergency room, doctor visits, immunizations, labs, and x-ray but does not provide long-term health care programs.
ALTCS, which falls under AHCCCS, is the Arizona Long-Term Care System. As its name indicates, it covers expenses for long-term health care, like nursing facilities, assisted living, and in-home care costs.
What is Long-Term Care?
Long-Term care includes Activities of Daily Living (ADLs), such as bathing, dressing, eating, etc., and Incidental Activities of Daily Living (IADLs), like laundry, shopping, housekeeping, etc.
When seniors cannot carry out daily living tasks independently, these services help them live as safely as possible. Long-Term care can be provided in the home or other facilities like adult day care centers, nursing homes, or assisted living communities, where onsite caregivers help the residents.
Who may need Long-Term Care?
Aging is the leading cause of the need for long-term care.
- 70% of all Americans are expected to need long-term care at some point in their (National Academy of Elder Law Attorneys)
- For a couple turning 65, there is a 75% chance that one of them will need long-term care. (The Wall Street Journal)
- Over 70% of people with Alzheimer’s live at home and receive 75% of the assistance they need from unpaid (Understanding Alzheimer’s, Alzheimer’s Association)
- The average annual cost of a private room nursing home in Arizona was $109,026 in 2021 and is expected to jump to over $191,000 by 2040. (Genworth – Annual Cost survey)
- 63% of caregivers use their own retirement and savings funds to pay for care for another person. (Genworth – Beyond Dollars 2018)
Many physical and mental changes occur as people age, affecting their ability to perform specific tasks or even care for themselves.
Are ALTCS and Medicaid the same thing?
Medicaid is a health care program jointly funded by the federal, state, and county governments and administered by the individual states.
Arizona Medicaid program is called the Arizona Long-Term Care System or “ALTCS.” Pronounced ALL-Tex.
The Medicaid department responsible for providing long-term care to Arizona seniors and disabled persons is the “Arizona Long-Term Care System, ALTCS,” or Arizona Medicaid.
So have dubbed ALTCS to mean “Arizona Long-Term Care for Seniors,” but this is not entirely accurate because you can be 18 years old and be approved for ALTCS.
Who Is Eligible to Apply for the ALTCS?
- Arizona residents ages 65 or above and those who are permanently disabled or impaired person.
- Be an Arizona resident (physical presence and intent to stay in Arizona)
- You must be able to show that you have applied for all other available benefits, such as pensions or Veterans Pension with aid and attendance benefits
- Reside in an ALTCS-approved facility or in your home
- You must be a U.S. Citizen or lawful resident alien
For ALTCS purposes, a resident is someone who is in Arizona even for just one second but doesn’t intend to return previous home state.
So just being in Arizona can make you eligible to apply.
What are the 2024 medical eligibility requirements for ALTCS
There were no changes in the requirements in 2024. To meet the medical eligibility requirements for ALTCS, a beneficiaries’ medical eligibility is evaluated by a process called Pre Admission Screening (PAS).
A sixty-point PAS score must be met to be ALTCS Medically Eligible.
The person applying must be at the care level given in an intermediate-level nursing home. Note that care can be provided in a person’s private residence.
This means they need help with dressing, bathing, getting up from a bed or chair, walking, grooming, eating, and going to the bathroom.
Being cognitively impaired will score if diagnosed by a neurologist.
Medical qualification is determined in a step-by-step process. Social workers or a nurse evaluates applicants by looking at their medical history, performing in-person or over-the-phone interviews, and assessing the applicant’s capacity to carry out activities of daily living. The ALTCS applicant must score 60 points to qualify.
A family member of the applicant or his legal representative may participate during the interview.
Being diagnosed with Dementia does score high, and they are more likely to become eligible for ALTCS.
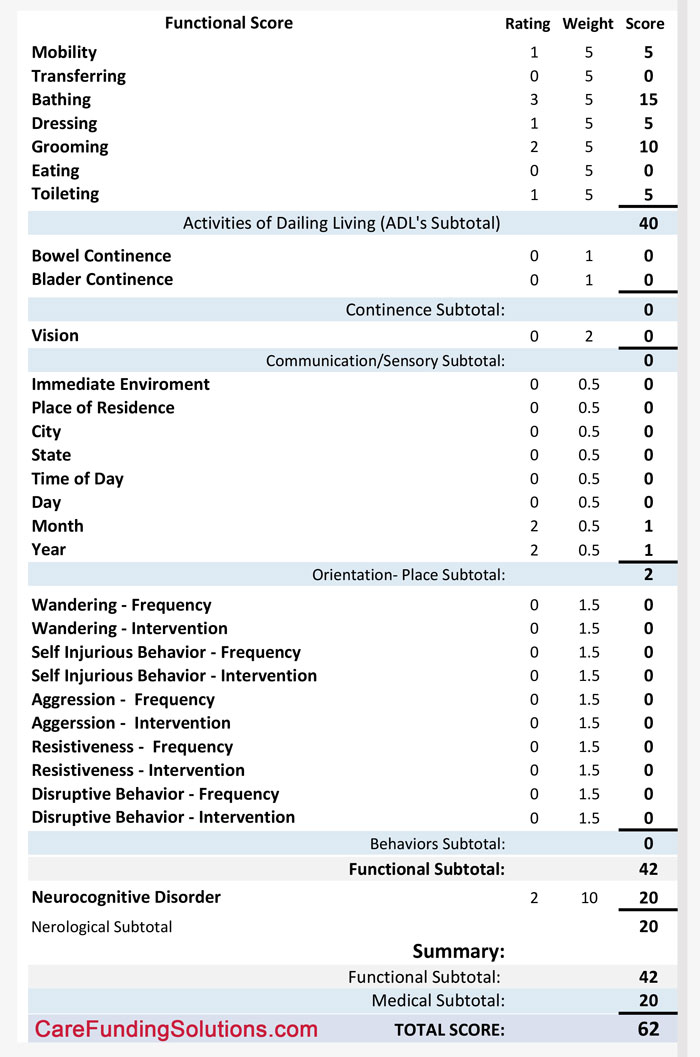
Below is a sample scoring chart; there, you can see the various ADLs and how they are scored.
What are the 2024 ALTCS financial requirements?
Here are the 2024 ALTCS financial qualifying requirements.
2024 ALTCS Income Limits:
- $2,829.00 per month for a single beneficiary
- The monthly income for a married applicant is $2,829.00, or $5,658.00 for both spouses.
ALTCS uses gross income before taxes and other deductions, including Medicare Part B and D premiums. Applicants are often denied because they learn that they
This isn’t very clear for married couples because the spouse not applying for Arizona Medicaid can have unlimited income. Meaning just that they could have $100,000 per month income, and the spouse needing care can still qualify if their income is below the limit or $2,829 per month.
So then, when does the $5,658 ALTCS income limit pertain to the qualification requirements for income?
The income is added together for a married couple and if the joint income is below $5,658 then the applicant can be approved without using an “Income Only Trust” or Miller Trust.
In my Arizona Medicaid book, “The Complete Arizona Medicaid and Veterans Pension Benefits Guide,” I explained the income rule in depth.
( https://carefundingsolutions.com/book )
Note that an “Income Only Trust” may satisfy the eligibility requirements for applicants whose gross limits.
Limits on Accountable Resources:
- An applicant: $2000
Community Spouse Resource Limits for Married Applicants:
- $30,828.00 Standard for Minimum Resource
- $154,140 is the Standard for Maximum Resource
Like the income cap for married couples, the Community Spouse or spouse not applying for benefits can be confusing too.
In order for the Community Spouse to be able to have $154,140 and still qualify, the household assets to have to be double that or $308,280.
So take a married couple with only $120,000, then the Community Spouse could only keep $60,000 and the spouse needing care $2,000. So they would need to convert or spend-down $58,000 to qualify.
Notice I wrote “convert” first and spend-down second.
Converting a countable asset to a non-countable asset is what the “Smart” do.
A “Smart Person” also does not try to do this without the help of a “Certifed Medicaid Planner.
Non-Countable Resources:
Non-countable assets include the primary residence in Arizona (the applicant’s home equity limit is $713,000.00), one vehicle, personal property, home goods, specific burial accounts, and Special Needs Trusts for disabled people below the age of 65.
See my book for a complete list of countable and non-countable resources/assets. “The Complete Arizona Medicaid and Veterans Pension Benefits Guide.” ( https://www.amazon.com/dp/B0BHL33HPN )
You will also find some conversion strategies in my book too.
How do I qualify for ALTCS benefits if income exceeds the required limit for ALTCS?
A Miller Trust or Income Only Trust can be used to qualify for ALTCS. Some states refer to this type of trust as a QIT or Qualified Income Trust.
Certified Medicaid Planner/ Legal Document Preparer Cecilia Dabbs, CMP™, can assist and guide the members about Miller Trust, helping them to be eligible to qualify for ALTCS.
When should someone start getting ready for ALTCS eligibility?
Planning is key to ensuring a successful outcome when you need long-term care. Multiple strategies can be employed, but many work best when the applicant is not in a care crisis.
You can better prepare me for the financial and medical requirements by planning ahead.
Examples of pre-planning or preparing to go on to ALTCS.
- Someone with Dementia should get an up-to-date exam and diagnosis from a “Neurologist.”
- Doctor records need to show the need for care. See your doctor and be sure they add notes that you need help with bathing because you are a fall risk, Eating because you are a choking risk, Decreasing because you have severe arthritis and can not button a button, and so on.
- You sold a home three years ago. ALTCS will want copies of the closing paperwork.
- Gather explanations of any unexplained banking transactions, like Check Number 1022 for $400, on the bank statement within the past five years.
- Be sure that your loved one doesn’t have any large gifts to a family member. Be prepared to disclose this. ALTCS will find it either way!
These are just a few everyday items that come up during the application process. So the sooner you meet with a “Certified Medicaid Planner™,” the better prepared you will be and the better outcome.
How long does it take to get ALTCS approval once an application has been submitted?
Generally, it takes between 60 and 90 days to get approval for ALTCS. Nearly 80% of applications are denied because they don’t meet the required criteria or because of minor mistakes the applicants make while applying for ALTCS.
But it can take much longer if you have a trust document in place of any kind. ALTCS’ Policy Department will scrutinize the trust.
The Policy Department doesn’t seem to have any urgency to do anything, and they can delay approval for several months.
Here is where a Certified Medicaid Planner is very helpful. They can keep on top of the application process and anticipate pitfalls and problems, which will help to speed up the process.
For ALTCS planning, is it necessary to hire an elder law attorney?
Particularly in Arizona, there is no need to hire an elder law attorney for ALTCS planning.
A Certified Medicaid Planner™ – CMP™ can help you through the entire process.
A Certified Legal Document Preparer Program, or CLDP, can assist Arizona residents who want to obtain ALTCS benefits but may need certain legal documents to qualify, like an “Income Only Trust” or Miller Trust.”
A Certified Legal Document Preparer – CLDP can also prepare a “Special Needs Trust” or Special ALTCS Qualification Trust or A SAQT Trust.”
Steve Dabbs is a CMP™, and Cecilia Dabbs is both a CMP™ and A CLDP.
Will ALTCS take my house if I am on ALTCS?
First, ALTCS will never take someone’s home away from them. Period!
However, they can place what is called a TEFRA lien on the home. A TEFRA lien is only for what ALTCS paid for care and no more. And the TEFRA lien is executed after the home is vacated and sold, never before!
ALTCS will never evict someone to recover what they paid.
Let me explain if the beneficiaries’ income is, say, $2,500 a month net after part b and other allowances like the personal needs allowance of $141.45.
And the cost for a semi-private room is $3,500, then ALTCS is only paying $1,000 per month after the share of cost. ($3,500 – $2,500) or $1000.
So let’s say that the applicant has been in assisted living for four years. That is the $48,000 that ALTCS paid.
A TEFRA lein of $48,000 would be placed on the home.
So when YOU decide to sell the home, the $48,000 is paid back to ALTCS. Think of it as an interest-free loan on steroids.
Why on Steroids? Because if you were not on ALTCS and privately paying for care, you are paying for retail costs for care, not effectively wholesale costs.
This would likely force you to sell your home and use the money to pay for care.
So that is what I mean by a zero-interest loan on steroids.
What is Spend-Down?
I call this asset conversion, not spend-down.
When someone is over-resourced, they must reduce or convert assets below the limit or spend-down their assets.
Understand you do not have to spend the assets on care to accomplish the reduction or spend-down.
Several conversion strategies allow you to convert a countable asset to a non-countable one or, again, Spend-Down.
This, once again, is where a Certified ALTCS Planner or Certified Medicaid Planner can assist. They can advise you on many conversion strategies to reduce (spend-down) and preserve your assets.
Is ALTCS just available to individuals who require care in a skilled nursing facility in Arizona?
No! ALTCS offers a wide range of care facilities and is not limited only to skilled nursing homes.
For persons reluctant to leave their residence, a home care agency may help them enjoy complete and secure health services.
Adult daycare centers allow seniors to become more socially interactive. Arizona Long Term Care System also provides services for those living in assisted living homes.
What are the differences in medical care quality between ALTCS members and those who pay out of pocket for their health care expenses?
ALTCS requires that care providers treat their beneficiaries like those privately paying for care in the same facility.
Meaning members of the Arizona Long-Term Care System are treated with the same respect and care as people who pay for their medical expenses. Arizona state law requires that ALTCS beneficiaries are treated equally and without discrimination, no matter their financial condition.
Legally the facility is not allowed to disclose to others who is on ALTCS and who is not.
When an ALTCS member qualifies for Medicaid, how do they start getting benefits?
It’s a step-by-step process that does not end when someone has been approved for the ALTCS program.
Once approved for the ALTCS benefits, the new member chooses a “Program Contractor” who will designate them as a Case Manager.
Currently, the program contractors are:
- Mercy Care
- Banner Health
- United Health Care
Case managers who work for one of the program managers create care plans. This is done with the help of the caregivers for approved members. A detailed discussion with the member and their family is helpful in developing the most appropriate health plan.
To reduce their own expenses, new members choose ALTCS-covered healthcare providers and facilities in collaboration with the case manager to benefit the most from ALTCS.
Ultimately, the Case Manager finalizes and approves the ALTCS services for the new member, so they start availing themselves with no further delay!
Can ALTCS members continue seeing their doctor?
Yes, ALTCS Members can keep their doctors, and they do not have to change their health plans, but……
There are some definite rules, and members must follow them if they want full coverage of ALTCS.
ALTCS only covers expenses for in-network doctors and not for out-of-network doctors.
However, members of the Arizona Long-Term Care System may see physicians who are not in their network, but they will have to pay from their own pockets.
But most members adopt a smart approach and choose a contracted doctor to save on this avoidable expenditure. In such cases, the Case Managers can assist new members in locating a new doctor they feel at ease with.
Can an ALTCS member use extra money to add health care services or benefits not provided by Arizona Medicaid?
While having medical services under the ALTCS program, approved members fully enjoy the needed and quality health facilities. Generally, there is no need to pay for additional benefits.
However, there is no restriction on it either. Members can pay from their own pockets in order to receive more benefits.
But it can risk their eligibility requirement for ALTCS as paying more is possible only due to an increased income or wealth. But a family member can pay for these.
This is why a gifting plan to qualify for ALTCS is truly smart. This sets aside money for just this purpose.
Working with a Certified Medicaid Planner can help to design a plan that will work best for the ALTCS beneficiary
What are the Non-Medical benefits offered by ALTCS?
ALTCS is not only bound to provide medical aid. It covers a wide array of non-medical assistance as well. ALTCS covers all activities of daily living (ADLs). Home health care, food delivery, changes to homes, adult home care, assistance with regular chores like bathing, laundry, and behavioral care assistance are some examples of non-medical facilities.
Do the ALTCS applicants have to use up all of their resources to qualify for the program?
The person applying must have countable resources below the limit of $2,000.
With that said, there are ways with proper Medicaid planning to preserve assets and still qualify for ALTCS long-term care benefits.
Converting countable assets to non-countable is one strategy. Another strategy is to use a gifting strategy in a combination of a particular type of annuity designed to convert a countable asset to a non-countable income.
This strategy works for both single and married applicants. However, it works particularly well for married individuals.
A Certified Medicaid Planner can help to develop a custom plan.
As I often say, “ALTCS is not just for the impoverished it is for the SMART, too”
To qualify for ALTCS benefits, is it allowed to transfer assets?
Gifting or transferring assets to qualify for ALTCS is not illegal.
It causes a Period of Ineligibility (POI) . The Divestment Penalty Divisor ( DPD) determines this period of ineligibility. The current 2024 Divestment Penalty Divisor or ( DPD) is $7,867.16 in Maricopa County and $7,281.17 in the rest of the state.
The DPD is divided into the Gifted Amount (GA). Simple formula { GA ÷ DPD = POI }
So take a single individual in Maricopa County that has $70,000. They are allowed to have $2,000 and must convert $68,000.
So if you take the gift or $68,000 and divide it by the 2024 DPD or $7,867.16 (if in Maricopa County Arizona), this equals 7.63 ($68,000 ÷$8,912.70 = 7.63)
So this means that coverage will begin in a little over seven and a half months.
Another way to gift and still have funds to pay through the penalty period is to purchase a Medicaid Compliant Annuity. Again this is explained in depth here. https://carefundingsolutions.com/medicaid-compliant-annuity-arizona/
And in my book: https://carefundingsolutions.com/book/
What is the current lookback period for ALTCS uncompensated transfers?
Currently, ALTCS examines each transfer an applicant has made going back five years from the date of their application. ALTCS looks at the applicants’ assets, income, and asset transfers made in the last five years.
ALTCS uses the AVS System or Asset Verification System. The AVS allows a state ALTCS worker to see the banking beginning and ending balance of Federal Bank Accounts.
What are Home and Community-Based Services or HCBS under ALTCS?
ALTCS provides a complete array of health services to its approved beneficiaries and pays for the cost of both home and community-based facilities. Some of the ALTCS home and community-based services include;
- Adult Daycare
- Homemaker Services
- Home Care
- Home Health Care
- Personal Care
- Assisting living
- Skilled nursing facility
- Adult daycare centers
- Mental health facilities
- Medical Transportation
- Behavioral health solutions
Does ALTCS decide where its approved members will live and where they will receive ALTCS benefits?
No, it’s all up to the qualified member or legal person representing the beneficiary. A consultation with the Medicaid Planner and a detailed discussion about the applicant’s medical health, can help the care recipient determine the residence and services he/she is going to have. If they receive care outside of their homes, their place of residence must be covered by ALTCS.
How much are caregivers paid under the ALTCS program?
ALTCS caregivers are paid the state minimum wage. Usually, the work duration assigned by ALTCS in a week is 30 to 40 hours. The Arizona Long-Term Care System strictly limits and ensures that caregivers are not paid for working more than 40 hours per week.
Does ALTCS compensate the spouse of the approved beneficiary as their caregiver?
ALTCS policy permits the spouse of a care recipient to be compensated as their caregiver, but they must satisfy certain requirements. In terms of proper training and qualifications, the spouse needs to meet the same standards as official caregivers. If they fail to meet this criteria, it will be difficult for them to be assigned as caregivers. Because ALTCS makes sure its members receive the safest and most appropriate health services.
The Case Manager or Program Contractor for ALTCS can direct and assist the spouse to meet these requirements. When the spouse has obtained the required training and is ready to serve, the Program Contractor then approves the spouse to start his duty as a caregiver.
Does ALTCS pay the cost of Assisted Living?
HCBS, or Home and Community-Based Waiver program in Arizona, allows individuals to stay in the home or get services in an Assisted Living community or home. There are a number of community-based facilities approved by ALTCS. So, Arizona Medicaid pays the cost of ALTCS-approved assisted living facilities in addition to home care services.
You can find a list of approved homes at https://ALTCS.org
How much do I have to pay for care once I am approved for ALTCS?
The amount you have to pay is called the share of the cost. I call it a co-pay.
The co-pay is based on your income minus the Personal Needs Allowance of $141.45 and any other Medicare and Medicare supplement premiums too.
A Community Spouse can also receive the Minimum Monthly Maintenance Allowance or MMMA. For 2024 the MMMA is $2,465 per month. They can also get a utility allowance and housing allowance which brings the total or Maximum Monthly Maintenance Allowance to $3,853.50 per month.
Take a Married Couple; the spouse needing care income is $3,000 per month, and the Community Spouses income is only $900 per month. There is not need for an “Income Only Trust,” because the total household income is only $3,900 per month, below the $5,658 limit.
But what about the co-pay for care?
Here the Community Spouse’s income is $900, but they are entitled to the MMMA of $3,715.
So, where is the $2,815 shortage coming from? It comes from the spouse’s income of $3,000. Leaving only $185.00 for a co-pay.
Now subtract the Personal Needs Allowance of $141.45 from the $185.00 remaining income after the MMMA calculation, and the co-pay would be $47.90!
It could be zero if the applicant has a Medicare Supplement plan.
Of course, every case is different so that the co-pay will vary. Also, if single or married will affect the amount of the co-pay too.
Why do so many applicants get denied by ALTCS?
Many do not qualify medically, which is the main reason for not being eligible. A person must be at a near-nursing level of care to qualify and score 60 points on the PAS exam.
The other main reason is over-resourced when they apply. This seems a no-brainer; you are either below the limits or not. If not, convert the assets and then apply.
Then there is the paperwork and deadlines that are a part of the application process. Many miss deadlines or do not provide the requested items, so ALTCS denies the application.
What is Estate Recovery?
Federal law requires that each state has a recovery program in place, AHCCCS administers the recovery program.
The recovery program is called “The Arizona’s Recovery Program.” The program is administered by a contractor, the Health Management Systems – HMS.
“HMS may impose a TEFRA lien on behalf of AHCCCS, as authorized under 42 U.S.C. 1396(p) (Tax Equity and Fiscal Responsibility Act of 1982) against all real property, including the member’s primary residence, of certain permanently institutionalized nursing home members.”
Source: State of Arizona Medicaid Estate Recovery Program DE-810 (Rev. 05/2022)
Recovery is for beneficiaries over age 55.
A TEFRA lien is only placed on a beneficiary once they are in a medical institution for 90 days, and it is determined that they are not likely or expect to return home.
If the beneficiary’s health improves, the TEFRA lien is lifted.
How much does Medicare pay for long-term care?
In a word. Nothing! Nada! Zip!
I’ve said that to people, and they have responded with, “They paid mine!”
The problem with that answer is they are confused with what was actually paid for by Medicare.
If you go to the “Medicare and You 2024” book see pages:
Page 25: What does Part A cover? It reads Inpatient care in a skilled nursing facility (not custodial or long-term care)
Page 27: Under the Inpatient Hospital Care and Long-Term Care Hospitals
In each Benefit Period, you pay:
- Days 1–60: Nothing after you meet your Part A deductible.
- Days 61–90: A $400 copayment each day.
- Days 91–150: A $800 copayment each day while using your 60 lifetime reserve days
I think this is where the confusion begins because someone is in the hospital for a 3-midnight stay and is sent to a Re-Hab Facility and they are there for only 45 days, and yes, Medicare paid for this.
But as soon as they are released and moved to an Assisted Living Facility, payments stop.
Page 28: Medicare only covers these services after a 3-day minimum medically necessary inpatient hospital stay. Some Medicaid Advantage Plans waive the 3-Day stay rule.
What is a Pooled Trust?
A pooled Trust is a type of Special Needs Trust pursuant to 42 U.S.C. 1396p(d)(4)(C)
A (d)(4)(C) Pooled Trust is formed by and administered by a non-profit organization. A separate account is set up for each individual.
One of the big advantages is the reduced admin cost.
A (d)(4)(C) Pooled Trust, is often used to allow someone that is on ALTCS to remain eligible if they receive additional assets due to a divorce or lawsuit settlement.
Funds can be used to pay for medical needs like dental that is not covered by Medicare
Once the ALTCS beneficiary passes, funds in the trust are used to pay back what the State of Arizona has paid for care.
What are the signs that indicate one is in need of long-term care or assisted living?
Here are some signs that may indicate that you or your loved one is in need of long-term care;
- Unclean house
- Hygiene problems
- Loss of or issues in mobility
- Gradual or sudden decline in memory
- Disturbing or upset mood
- Frequent body aches
- Problem in driving
- Decrease response or unopened mail
- Hiding mental and health issues
- Frequent hospital stays in a short time
- Changes in feeding habits and weight loss
- Feeling lonely
- Moldy kitchen items
- Many falls in a brief period
- Increase health issues
Is there a way to be pre-approved for ALTCS?
Well, sort of, technically, no, but you can be ALTCS-approved before you move into a care home or facility.
We often get someone pre-approved so that they do not have to worry about how they will pay for needed care, before they move from their home to a facility.
This is important for many; our Certified Medicaid Planners can help with this process.
Who should hire an Attorney or “Certified Medicaid Planner™?
1: Your assets and/or income are above the limits
2: You have been denied benefits.
3: You want to preplan
Call us at 480-967-8477 or complete the form below.
